Blog post -
The Importance of Early Warning Scores in Identifying Deteriorating Patients
There is now overwhelming evidence that significant numbers of patients are harmed from the healthcare they receive resulting in permanent injury, increased length of stay in hospital or even death.
It is now widely accepted that 1 in 10 patients admitted to hospital will be unintentionally harmed in some way. Some of these adverse events will be inevitable complications of treatment, however, at least half of these events are thought to be preventable.

In the UK, reviews of case records have shown that in 2014 there were 1.2 million reported care incidents and 12,000 avoidable deaths.
It is vital that changes are made to reduce these figures and providing clinical staff with the tools they need to be aware of those patients who are deteriorating fast will be a significant step forward. This is particularly true when patients are transferred across acute and community settings, for example from GP or ambulance to a hospital emergency department.
Early Warning Scoring (EWS) systems provide a commonly understood way to recognise the degree of deterioration (or improvement) in a patient’s status, and can therefore, ensure that every patient is seen at the right time by the right person. The EWS is based on the collection of a combination of vital signs including heart rate, respiratory rate, oxygen saturation, blood pressure and body temperature.
Fantastic work has already been done in healthcare settings around the UK, including the “Safer Care through Early Warning Scores” programme which was launched to achieve a single EWS right across the West of England. It was agreed that the adoption of the National Early Warning (NEWS, Royal College of Physicians) would help to quickly and consistently determine the degree of a patient’s illness, wherever treatment takes place in the West of England. This EWS system alerts to the onset of adverse physiological events, enabling medical teams to act faster and deliver adequate care to patients before the occurrence of severe complications. One of the most innovative aspects of this programme is that the NEWS score is used not only in the hospital but has been adopted as the criticality measure for patients at all stages of their journey across primary care, ambulance transportation, emergency and acute care.

Another example of good practice is in Wales where the NEWS systems has been introduced and rolled out to clinical areas throughout the country to bring service and health care improvements and reduce harm to patients.
EWS systems were first introduced for in-patients in hospitals where patients in general wards have their ‘obs’ taken at intervals (typically 4 to 8 hourly) and recorded on a clinical chart. Between “obs” significant negative changes in a patients’ status can occur. Such infrequent monitoring (and consequent sparse data points) makes it almost impossible to identify trends that might have been able to predict the patient’s deterioration. Patients can also sometimes deteriorate quickly in between observations and it’s vital that this is deterioration is picked up quickly.
Technology can play a huge part in helping hospitals and healthcare organisations use EWS to identify deteriorating patients and support intervention before patients suffer adverse events.
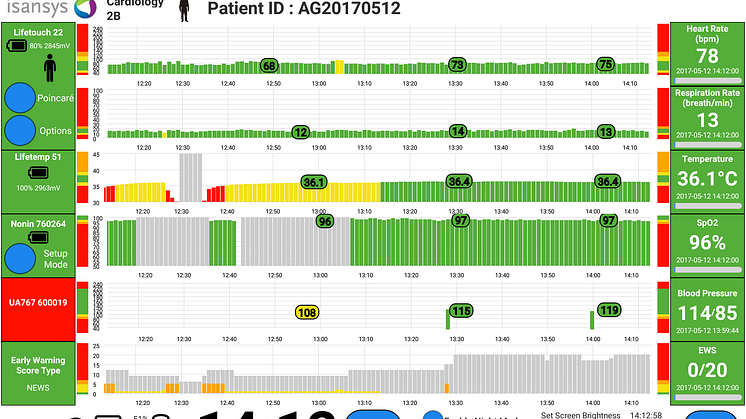
At Isansys Lifecare, we have developed the Patient Status Engine (PSE) - a complete system that can address in-hospital deteriorations and patient safety issues. The PSE is an innovative, continuous, vital sign data acquisition, analysis and prediction platform that combines unobtrusive wireless wearable sensors, wireless networks, analytical algorithms and big data to provide low cost, continuous, high resolution monitoring for all patients in hospital, and at home.

The PSE can address in-hospital deterioration's and patient safety issues
The PSE uses wireless body-worn sensors to automatically collect and analyse those vital signs used for NEWS scores (heart rate, respiration rate, temperature, oxygen saturation and blood pressure) and additionally provides manual data entry screens for rapid and simple capture of coma and pain scores as required. The system collects precise, high resolution and continuous patient data and provides an accurate real time, continuous NEWS score as the default EWS for adult patients. The NEWS chart and score for each patient is displayed at the bedside, and also delivered to the nurse station and to any authorised connected device such as a smart phone or tablet carried by nursing or clinical staff.

This new technology is already being used as part of a ground-breaking research study, RAPID (Real-Time Adaptive & Predictive Indicator of Deterioration) at Birmingham Children’s Hospitalwhich aims to predict deterioration in seriously ill children through the development of an innovative, self-learning, personalised EWS for paediatric patients.
Keith Errey, CEO of Isansys, says: “There is a pressing need to improve patient safety, the way patients are monitored and how patients’ data is collected and analysed. Remote monitoring systems that use wireless connectivity, wearable sensors and information technologies to collect and analyse patient data are the future of patient monitoring and will enable medical professionals to deliver better care, improve patient safety and increase efficiencies. These technologies by providing the means for automatic vital sign data capture and delivering real time EWS for any (or all) patients cost effectively and at large scale, will also help reduce the costs associated with avoidable patient deterioration, medical errors, readmissions to intensive care wards and admissions (and readmissions) to hospital. In the future they will also play a major role in engaging patients in their own care.”
Isansys is also working with Sorlandet Hospital in Norway to implement the PSE in three hospitals. As a cutting-edge technology hospital, Sorlandet Hospital is aware of the positive impact that wireless monitoring technology may have on the early detection of patients’ deterioration.
Line Pedersen, who is leading the project, says: “This is an important project to improve patient safety. I believe it can both reduce mortality and save the hospital money.”
The Canberra Hospital in Australia recently carried out a study to determine whether the introduction of a multi-faceted intervention (newly designed ward observation chart, a track and trigger system and an associated education program) to detect clinical deterioration in patients would decrease the rate of adverse outcomes.
During the study they found that the implementation of EWS showed a reduction in unplanned admissions to ICU from 1.8% to 0.5%, a decrease in unexpected hospital deaths from 1% to 0.2% and a reduction in all hospital deaths from 2.6% to 0.6%
The study also investigated the implementation of EWS in primary care and found that it is adequate to trace elderly patients in need of medical assistance. At a score lower than two, 24% of patients were visited by a doctor and admitted directly to hospital, at a score more than five, this number increased to 45%.
In conclusion they discovered that simple, practical ward based intervention improves the process of recognising clinical deterioration in ward patients and potentially can improve patient outcome.
It follows then that deploying the Isansys Patient Status Engine platform to automate the process of patient data capture and generation of the EWS can only further enhance these results by removing the inconsistencies and inefficiencies associated with manual patient observations and data entry. The key objectives of a number of the current early stage deployments of the PSE are to quantify both the patient improvements and the healthcare economic benefits.

