Pressmeddelande -
LANDMARK OUTCOMES STUDY SHOWS THAT REPATHA (EVOLOCUMAB) DECREASES LDL-C TO UNPRECEDENTED LOW LEVELS AND REDUCES RISK OF CARDIOVASCULAR EVENTS WITH NO NEW SAFETY ISSUES
- Repatha Significantly Reduces Risk of Hard Major Adverse Cardiovascular Events by 20 Percent
- Risks of Heart Attack, Stroke and Coronary Revascularization Were Nominally Reduced by 27 Percent, 21 Percent and 22 Percent, Respectively
- Patients in Study had History of Heart Attack, Stroke or Symptomatic Peripheral Arterial Disease and Were Treated With Optimized Statin Therapy
- Detailed Results Simultaneously Published in the New England Journal of Medicine and Presented at the American College of Cardiology 66th Annual Scientific Session
THOUSAND OAKS, Calif. (March 17, 2017) - Amgen (NASDAQ:AMGN) today announced that the 27,564-patient Repatha (evolocumab) cardiovascular outcomes study, FOURIER, established for the first time that maximally reducing low-density lipoprotein cholesterol (LDL-C) levels with Repatha, beyond what is possible with the current best therapy alone, leads to a further reduction in major cardiovascular events, including heart attacks, strokes and coronary revascularizations.
The study was statistically powered around the hard major adverse cardiovascular event (MACE) composite endpoint of first heart attack, stroke or cardiovascular death (key secondary composite endpoint) and found that adding Repatha to optimized statin therapy resulted in a statistically significant 20 percent (p<0.001) reduction in these events. The robust benefit in this objective measure started as early as six months and continued to accrue through the median 2.2 years of the study. In fact, the magnitude of the risk reduction in the hard MACE composite endpoint grew over time, from 16 percent in the first year to 25 percent beyond the first year.
The study also found a statistically significant 15 percent reduction (p<0.001) in the risk of the extended MACE composite (primary) endpoint, which included hospitalization for unstable angina, coronary revascularization, heart attack, stroke or cardiovascular death.
Patients on Repatha experienced a reduction in the risk of heart attack (27 percent, nominal p<0.001), stroke (21 percent, nominal p=0.01) and coronary revascularization (22 percent, nominal p<0.001). Consistent with recent trials of more intensive LDL lowering, there was no observed effect on cardiovascular mortality.1-5 Similarly, there was no observed effect on hospitalization for unstable angina. In an exploratory analysis, the relative risk reduction for fatal and non-fatal heart attack or stroke was 19 percent in the first year (p=0.003) and 33 percent beyond the first year (p<0.00001).
“We now show for the first time in a dedicated outcomes study that decreasing LDL cholesterol with PCSK9 inhibition results in clinically meaningful cardiovascular benefit,” said Marc S. Sabatine, M.D., M.P.H., chairman of the TIMI Study Group, the Lewis Dexter, MD, Distinguished Chair in Cardiovascular Medicine at Brigham and Women's Hospital, and Professor of Medicine, Harvard Medical School, Boston. “These benefits were achieved with lowering LDL cholesterol down to a median of 30 mg/dL, which is well below current targets, and the magnitude of risk reduction increased the longer patients were on therapy. These results support the need for long-term, vigorous LDL cholesterol reduction in our patients with cardiovascular disease.”
When added to statin therapy, Repatha reduced LDL-C from a median of 92 to 30 mg/dL, a reduction of 59 percent at week 48, which was sustained throughout the trial. At 48 weeks, the LDL-C was reduced to at least 25 mg/dL in 42 percent of patients treated with Repatha, as compared with <0.1 percent in the placebo group (p<0.001). Additionally, treatment with Repatha had favorable effects on other lipid parameters.
“This is a game changer for high-risk patients. Even though these patients were optimally treated with the latest therapies, they were still at high risk for an additional cardiac event. It’s remarkable to see such a large impact in reducing cardiac events given that this patient population was only on Repatha for about two years,” said Sean E. Harper, M.D., executive vice president of Research and Development at Amgen. “The absolute benefit will be even greater than what we observed in the Repatha outcomes trial, since the cardiovascular event rate in clinical practice is about 2-3 times higher than what is typically reported in a rigorously controlled outcomes trial.”
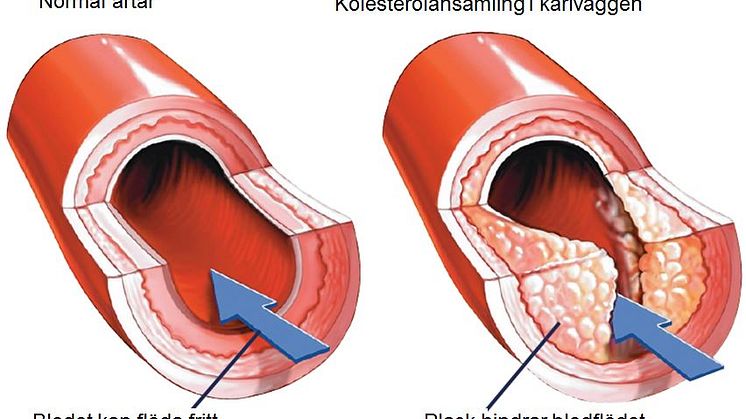
Repatha was developed from the breakthrough work of Amgen scientists who elucidated the interaction of PCSK9 and the LDL receptor (LDLR), including the site where the LDLR binds to PCSK9, and developed antibodies that bind to PCSK9 at that site and block the interaction of PCSK9 with the LDLR. These scientific advances resulted in the intellectual property to antibodies to PCSK9 that protect Repatha. An extensive set of clinical trials subsequently demonstrated the effectiveness of Repatha in lowering LDL-C, in regressing coronary atherosclerosis and finally now in reducing the risk of major adverse cardiovascular events. From its inception, the program has demonstrated the power of human validation of a drug target based on genetic insights, an approach which is playing an increasingly important role across Amgen’s therapeutic portfolio.
No new safety concerns were identified in this large clinical trial with roughly 60,000 patient-years of follow-up; this included the assessment of patients who achieved very low levels of LDL-C. In particular, there were no notable differences seen between treatment arms in the overall rate of adverse events, serious adverse events or adverse events leading to study drug discontinuation. Likewise, rates of adjudicated new onset diabetes (8.1 percent Repatha; 7.7 percent placebo), muscle-related side effects (5.0 percent Repatha; 4.8 percent placebo), cataract (1.7 percent Repatha; 1.8 percent placebo), neurocognitive adverse events (1.6 percent Repatha; 1.5 percent placebo) and allergic reactions (3.1 percent Repatha; 2.9 percent placebo) were similar between the two arms. Injection site reactions were more common with Repatha than with placebo (2.1 percent Repatha; 1.6 percent placebo). In the Repatha arm, post-baseline new binding antibodies were detected in 43 patients (0.3 percent) and neutralizing antibodies in none. Detailed results from the Repatha cognitive function study (EBBINGHAUS) will be presented in a separate Late-Breaking Clinical Trial Session on Saturday, March 18 at 9 a.m. ET.
Repatha Cardiovascular Outcomes (FOURIER) Study Design
FOURIER (Further CardiovascularOUtcomesResearch with PCSK9Inhibition in Subjects withElevatedRisk), a multinational Phase 3 randomized, double-blind, placebo-controlled trial, is designed to evaluate whether treatment with Repatha in combination with statin therapy compared to placebo plus statin therapy reduces cardiovascular events. The primary endpoint is the time to cardiovascular death, myocardial infarction, stroke, hospitalization for unstable angina, or coronary revascularization. The key secondary endpoint is the time to cardiovascular death, myocardial infarction or stroke.
Eligible patients with high cholesterol (LDL-C ≥70 mg/dL or non-high-density lipoprotein cholesterol [non-HDL-C] ≥100 mg/dL) and clinically evident atherosclerotic cardiovascular disease at more than 1,200 study locations around the world were randomized to receive Repatha subcutaneous 140 mg every two weeks or 420 mg monthly plus optimized statin dose; or placebo subcutaneous every two weeks or monthly plus effective statin dose. Effective statin therapy was defined as at least atorvastatin 20 mg or equivalent daily with a recommendation for at least atorvastatin 40 mg or equivalent daily where approved. The study was event driven and continued until at least 1,630 patients experienced a key secondary endpoint.
About Repatha (evolocumab)
Repatha® (evolocumab) is a human monoclonal antibody that inhibits proprotein convertase subtilisin/kexin type 9 (PCSK9). Repatha binds to PCSK9 and inhibits circulating PCSK9 from binding to the LDLR, preventing PCSK9-mediated LDLR degradation and permitting LDLR to recycle back to the liver cell surface. By inhibiting the binding of PCSK9 to LDLR, Repatha increases the number of LDLRs available to clear LDL from the blood, thereby lowering LDL-C levels.6
Repatha is approved in more than 40 countries, including the U.S.,Japan,Canadaand in all 28 countries that are members of theEuropean Union. Applications in other countries are pending.
CONTACT: Amgen, Thousand Oaks
Kristen Davis, 805-447-3008 (Media)
Kristen Neese, 805-313-8267 (Media)
Arvind Sood, 805-447-1060 (Investors)
REFERENCES
- Cannon CP, et al. N Engl J Med. 2004;350:1495-1504.
- LaRosa JC, et al. N Engl J Med. 2005;352:1425-1435.
- Pederson TR, et al. JAMA. 2005; 294:2437-2445.
- Search Collaborative Group Lancet 2010; 376: 1658–69.
- Cannon CP, et al. N Engl J Med. 2015;372:2387-2397.
- Repatha® U.S. Prescribing Information. Amgen.
- 7.World Health Organization. Cardiovascular diseases (CVDs) fact sheet. http://www.who.int/mediacentre/factsheets/fs317/en/ Accessed March 2017.
Ämnen
About Amgen in the Cardiovascular Therapeutic Area
Building on more than three decades of experience in developing biotechnology medicines for patients with serious illnesses, Amgen is dedicated to addressing important scientific questions to advance care and improve the lives of patients with cardiovascular disease, the leading cause of morbidity and mortality worldwide.7 Amgen's research into cardiovascular disease, and potential treatment options, is part of a growing competency at Amgen that utilizes human genetics to identify and validate certain drug targets. Through its own research and development efforts, as well as partnerships, Amgen is building a robust cardiovascular portfolio consisting of several approved and investigational molecules in an effort to address a number of today's important unmet patient needs, such as high cholesterol and heart failure.
About Amgen
Amgen is committed to unlocking the potential of biology for patients suffering from serious illnesses by discovering, developing, manufacturing and delivering innovative human therapeutics. This approach begins by using tools like advanced human genetics to unravel the complexities of disease and understand the fundamentals of human biology.
Amgen focuses on areas of high unmet medical need and leverages its expertise to strive for solutions that improve health outcomes and dramatically improve people's lives. A biotechnology pioneer since 1980, Amgen has grown to be one of the world's leading independent biotechnology companies, has reached millions of patients around the world and is developing a pipeline of medicines with breakaway potential.
For more information, visit www.amgen.com and follow us on www.twitter.com/amgen.