Press release -
Key genes controlling brain tumour spread identified – may lead to new treatments
An international research team led from Uppsala University has identified new mechanisms behind how the aggressive brain tumour glioblastoma spreads in the brain. Targeting the identified connection between the tumour invasion routes and the tumour cell states could be a potential new treatment strategy.
Glioblastoma is the most common and most lethal primary brain cancer in adults, known for its capacity to spread locally in the brain rather than forming distant metastases. The locally infiltrating cells are largely out of reach for current therapies and it is therefore crucial to determine how the spread in the brain is controlled.
In the current study, which was recently published in the journal Nature Communications, the researchers found that some tumour cells choose to grow along blood vessels in the brain whereas others spread diffusely in the brain tissue. This choice is controlled by the tumour cell states.
“We combined single-cell profiling and spatial protein detection in both mouse models and tumour samples from patients. Depending on gene activity in the cells we could group them into different cell states and found a strong correlation between cell state and their invasion patterns,” says the study’s senior author Professor Sven Nelander at the Department of Immunology, Genetics and Pathology.
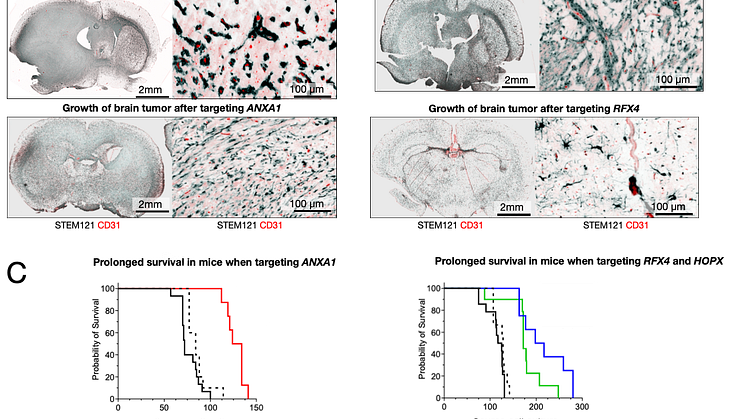
The researchers identified three key factors involved in controlling the invasion routes. The gene ANXA1 was linked to invasion along blood vessels while HOPX and RFX4 was associated with diffuse infiltration in the brain. To evaluate the role of the genes, the researchers tested to knock them out in preclinical models, which resulted in a shift in the tumour’s invasion pattern. In several cases, the survival of the experimental animals was also prolonged.
“Our findings show that glioblastoma is not a homogenous disease but is made up of several cell types with different invasion patterns. Understanding and controlling these patterns opens up for new targeted treatments,” says Sven Nelander.
The researchers also discovered proteins encoded by the identified genes in tissue samples from patients. In addition, they found that the presence of the ANXA1 and RFX4 correlated with poor survival. This indicates that these proteins could have a value as prognostic biomarkers.
The study was performed as a collaboration between scientists at Uppsala University, Queen Mary University of London, and Dana-Farber Cancer Institute in Boston.
Contact
Sven Nelander, Professor at the Department of Immunology, Genetics and Pathology, Uppsala University
Email: sven.nelander@igp.uu.se tel: +46 76-1380123
Doroszko et al. The invasion phenotypes of glioblastoma depend on plastic and reprogrammable cell states, Nature Communications, DOI: 10.1038/s41467-025-61999-1
Topics
Categories
Founded in 1477, Uppsala University is the oldest university in Sweden. With more than 50,000 students and 7,500 employees in Uppsala and Visby, we are a broad university with research in social sciences, humanities, technology, natural sciences, medicine and pharmacology. Our mission is to conduct education and research of the highest quality and relevance to society on a long-term basis. Uppsala University is regularly ranked among the world’s top universities. www.uu.se